Nearly Half of all Positive Blood Cultures are False Positives
Blood cultures are the ‘gold standard’ test for diagnosing sepsis yet approximately 40% of positive blood culture results are false positive due to contamination.24 These preventable errors can lead to the misdiagnosis of sepsis.
The Consequences of Misdiagnosed Sepsis
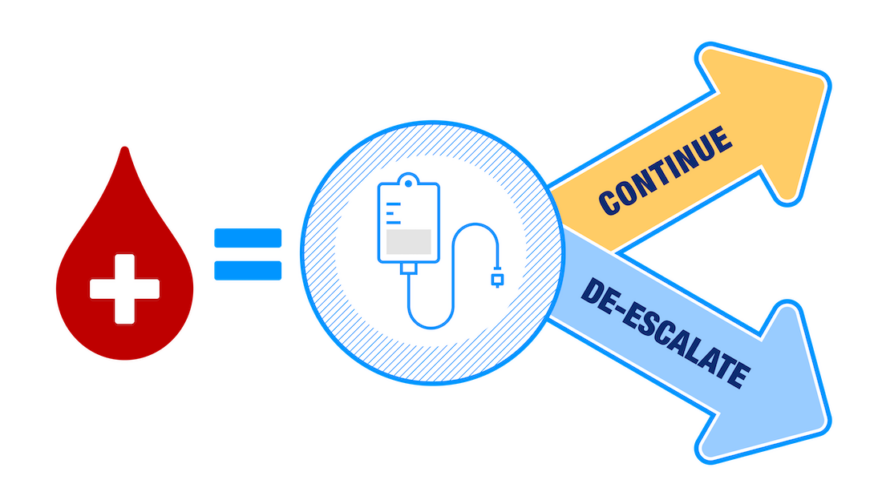
False-positive results present a major dilemma for clinicians: whether to continue or discontinue the patient’s antibiotic treatment.
Discontinuing therapy for a septic patient significantly increases morbidity and mortality rates, so clinicians may elect to continue antibiotics and observe the patient. However, when the patient’s results are false positive, they receive unnecessary broad-spectrum antibiotics that can extend hospital stay and exposure to secondary infections, such as Clostridioides difficile Infection (CDI), and other Hospital-Acquired Infections (HAIs).

Establishing the New Standard in Sepsis Testing Accuracy
We’re partnering with U.S. hospitals and healthcare providers to prevent sepsis misdiagnosis by improving the accuracy of blood culture results using Steripath®.
Steripath is FDA 510(k)-cleared with a specific indication to reduce blood culture contamination3 for sepsis testing accuracy. The submission included clinical studies reporting an 83% and 88% contamination rate reduction for blood cultures collected via peripheral venipuncture and peripheral IV start and peripheral venipuncture only.

We’re on a mission to improve the diagnostic accuracy and timeliness of sepsis test results.